Introduction: HLA-Haploidentical bone marrow transplant (haplo-BMT) is a curative approach for individuals with severe sickle cell disease (SCD) who lack an HLA-identical sibling donor. Haplo-BMT expands the donor pool among adults and children with SCD to > 90% and is a less toxic treatment option than myeloablative matched related donor transplant, gene therapy or gene editing. In 2013, our research team developed a multi-institution learning collaborative with the main objective of optimizing haplo-BMT. In a Phase II clinical trial, to improve engraftment rates, we augmented the original Hopkins haplo-BMT protocol (Bolaños-Meade et al. Blood 2012) with thiotepa (10 mg/kg). The trial was conducted at 3 sites and showed durable engraftment in 93% (14/15) of participants (including 2 with previous graft rejection), and a 100% overall survival after a median follow-up of 13.3 months (de la Fuente et al. BBMT 2019). We present results of extension of this ongoing trial comprising additional sites and participants.
Material and methods: The trial was approved by the Institutional Review Board (IRB) at each participating site and opened in October 2013 (ClinicalTrials.gov identifier NCT01850108). The global learning collaborative includes 22 sites, in 10 countries, meets weekly via conference calls for sharing of SCD Haplo-BMT knowledge and patient related questions. Each site has a standalone institutionally IRB protocol, with similar eligibility criteria, and data sharing agreement with Vanderbilt University Medical Center. The agreements for aggregate REDCap data sharing and DSMB assessment of the outcomes with stopping rules.
Common conditioning regimen included: rabbit ATG 4.5 mg/kg, thiotepa (10 mg/kg), fludarabine 150 mg/m2, cyclophosphamide 29 mg/kg and TBI 2Gy. GVHD prophylaxis included posttransplant cyclophosphamide (PTCy) 100 mg/kg, mycophenolate mofetil and sirolimus. Bone marrow mobilized with filgrastim (5-10 μg/kg/d x5 days) was initially used, 27% (11/41), but later stopped at several sites. Primary graft failure was defined as <5% donor myeloid chimerism or < 5% donor cells by whole blood chimerism by day +42 posttransplant. Secondary graft rejection was defined <5% donor myeloid chimerism or < 5% donor cells by whole blood chimerism with prior documentation of > 5% donor (myeloid) cells by day +42. The primary endpoint was 1-year EFS. Primary or secondary graft rejection, stroke, and death were considered events. Safety stopping rules were implemented, independent of age, using graft failure, death, grade III or IV acute GVHD or moderate or severe chronic GVHD.
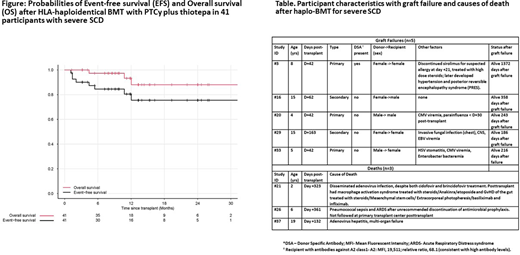
Results: We enrolled 41 consecutive participants from 8/14/2014 - 6/30/2020. Participant genotype included 39 patients with HbSS, 1 patient each with HbSC and Sβ0 thalassemia. Median age was 16.9 years (range 1.3 to 43), and 51% (21/41) of participants were <18 years of age. Donors included siblings (14/41, 34%), parents (27/41, 61%), and 88% (36/41) had sickle cell trait. Median TNC dose was 5.8 x 108 /kg (4.2, 8.0), and median CD34+ and CD3+ cell doses were 3.9 x 106/kg (2.6, 6.1) and 32.3 x 108/kg (27.1, 50.8), respectively. A total of 93% of participants engrafted. Median times to neutrophil (> 500/mcL) and platelet (>50 x 109/L) counts were 20 days (17.0, 24.2) and 32 days (27.0, 36.8) respectively. Incidence of grades III-IV acute and moderate chronic GVHD were 9.7% (4/41) and 12.1% (5/41), respectively. No participant had severe GVHD. Among durably engrafted participants, 81.8% (27/33) were off immunosuppression at 1-year posttransplant. Kaplan-Meier probabilities of EFS and OS were 75.5% (95% CI 61.3%, 92.9%) and 87.9% (95% CI 75.5%, 100.0%) at one year, respectively (Figure). Mortality was 7.3% (3/41). Graft failure was 12% (5/41; 3-primary and 2-secondary). All graft failures were in participants <18 years of age, and all had autologous reconstitution (Table).
Conclusion: Our novel global learning collaborative effort for haplo-BMT for SCD is a scalable and efficient approach to sharing knowledge and implementing curative therapy for SCD. Importantly all haplo-BMT candidate had donors. An unexpected outcome in this trial, not likely to occur by chance, is that all graft rejections occurred in young participants (< 18 years), and all older participants (> 18 years) engrafted. The trial will add new stopping rules by age strata (<18, > or = to 18 years) and will modify the conditioning regimen in pediatric stratum.
Black:HRSA: Research Funding; Pfizer: Research Funding; Novartis: Research Funding; Micelle BioPharma: Research Funding; NHLBI: Research Funding. DeBaun:Novartis: Membership on an entity's Board of Directors or advisory committees; Global Blood Therapeutics (GBT): Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal